Spontaneous Pneumothorax

Ms. Kate Burnand
Consultant Paediatric Surgeon,
St George’s Hospital, London
Background and Overview
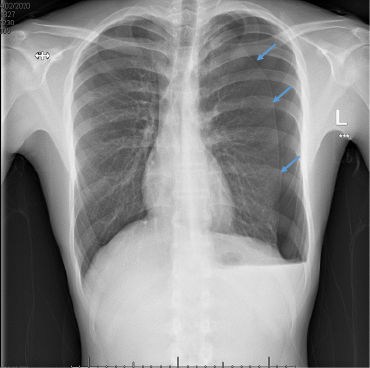
Primary spontaneous pneumothorax (PSP) occurs in those patients with no underlying lung pathology, whereas secondary spontaneous pneumothoraces occur in patients with pre-existing lung conditions (e.g. asthma, COPD, cystic fibrosis, infection, lung carcinoma etc.). It is rare and typically affects male adolescents and young adults. Within our paediatric population the incidence is probably about 3/100,000.
The vast majority of cases are due to ruptured sub-pleural blebs which for some reason seems to occur far more frequently in tall, skinny boys. The commonest presentation is that of sudden onset pleuritic chest pain and dyspnoea at rest. It is most unusual for a PSP to cause a tension pneumothorax, so the presentation is often mild and most have had symptoms for a few days.
Initial management will include oxygen and analgesia. High-flow oxygen speeds up resolution about 4x faster and is most pronounced in patients with a large pneumothorax. Simple aspiration ± chest drain may also be indicated. Recurrence rates are significant and somewhere between 10-50%.
For recurrent or complicated disease, the typical treatment is Video Assisted Thoracic Surgery (VATS) which might include apicectomy of the lung (using an endo-stapler) and mechanical or chemical pleurodesis. It may not be without complications including development of Adult Respiratory Distress Syndrome (ARDS) (~5%), persistent pneumothorax, haemothorax and recurrence (1-4%).
Areas of Controversy
-
Initial management – conservative, aspiration, chest drain
Guidelines from the British Thoracic Society (BTS) published in 2010 states that if the patient is: haemodynamically stable; the pneumothorax is unilateral and with a size >2cm or breathless then aspirate first. Only insert a chest drain if haemodynamically unstable, bilateral or there has been no improvement with aspiration.
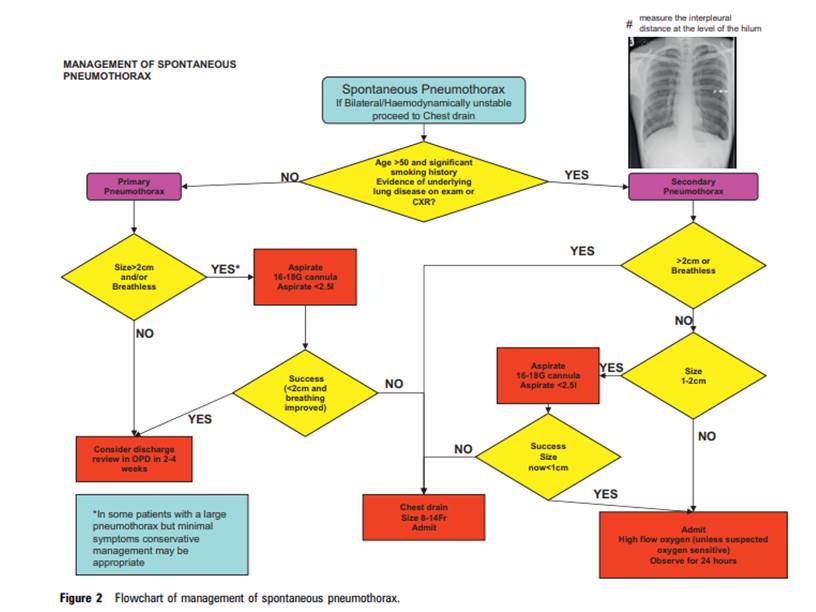
However, a RCT published this year in the New England Journal of Medicine (Brown et al. 2020) showed that even larger pneumothoraces can be successfully managed without aspiration or chest drain in the first instance providing that the patient remains haemodynamically stable, symptoms are controlled with oxygen and analgesia and on repeat CXR the PTx is not getting significantly bigger.
-
Imaging – Do we need to CT everyone pre-operatively?
| Advantages | Disadvantages |
| Helps with informed consent | May not change your management |
| Extent of disease – contralateral, apical portions of middle/lower lobe | If lung not re-expanded then may miss blebs |
| Assessment of secondary causes of pneumothorax – underlying disease, bullae, exotoses etc. | Not as sensitive as thoracoscopy for detecting blebs. |
Historically most surgeons have opted to get a CT scan prior to definitive surgery, and the table summarises some of the reasoning.
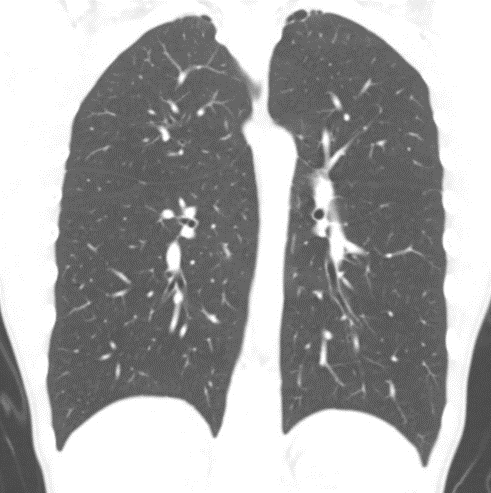
However, Shawn St Peter’s group in Kansas showed that the sensitivity of CT for identifying blebs was only 36% (Laituri et al. 2011) which diminishes its rationale.
Most surgeons will offer definitive surgery after the first recurrence of a pneumothorax with or without visible blebs on CXR or CT. Thoracoscopy/Thoracotomy is superior to CT for detecting blebs. Even when blebs are not visible macroscopically there have been histological studies that have demonstrated sub-pleural blebs in 100% of apical resections for PSP. Therefore, surgeons will commonly perform an apicectomy even in the absence of visible blebs. The staple line also allows the apex of the lung to stick better to the chest wall.
For barn door cases it has become the norm to move away from a universal CT scan for all patients.
-
When to offer surgery.
- 2nd ipsilateral pneumothorax
- 1st contralateral pneumothorax
- Bilateral spontaneous pneumothorax
- Persistent air-leak or failure of lung to re-expand 5 days after chest drain insertion
- Spontaneous haemothorax
not so applicable to children
- Professions at risk– e.g. pilots, divers
- Pregnancy
Recently a prospective multi-institutional pilot study in the USA (Leys et al. 2020) looked at simple aspiration of primary spontaneous pneumothorax as a predictive tool for need for definitive surgery (VATS). It recruited 33 patients over a 2-year period. Aspiration was performed using a ≤12 Fr catheter with suction with a CXR performed immediately after.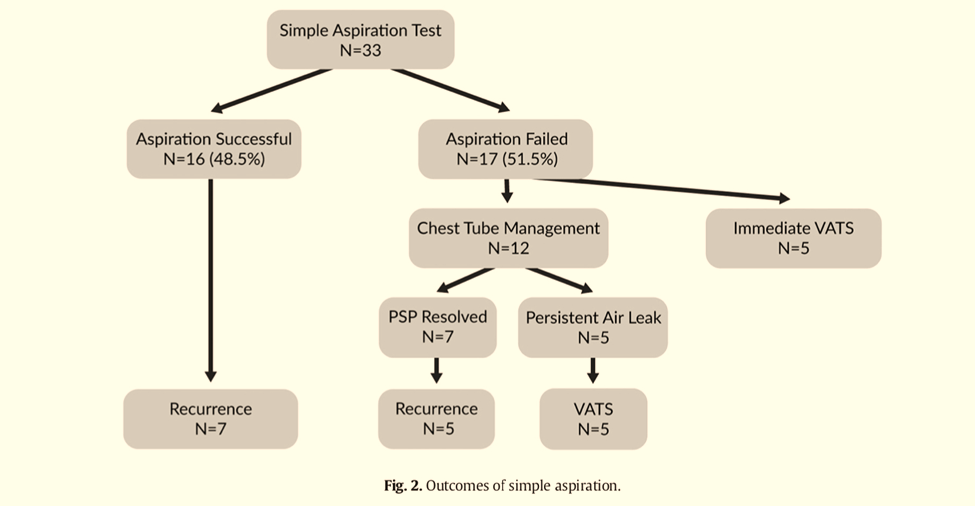
- SUCCESS – lung re-expanded (apex above 4th rib, rim of residual PTx no lower than top of 6th rib), child remained well for 6 hours – then could be discharged
- FAILURE – PTx enlarged or did not adequately expand, patient developed or had ongoing clinical signs
Conclusion: Simple aspiration test upon presentation with PSP predicts chest tube failure with 83% positive predictive value.
-
Surgery – unilateral or bilateral?
Most surgeons (70%) according to a US poll (GlobalCastMD) would only operate on a symptomatic side even with evidence of blebs on the contralateral side on a CT scan. There is also no evidence that blebs can predict if someone will develop a PTx on the contralateral side.
If a patient has bilateral synchronous symptomatic pneumothoraces then the jury is out as to whether to take on both sides simultaneously. The concern is that a bilateral VATS with apicectomy and pleurodesis is more painful and there is an increased chance of developing ARDS. In order to reduce the chance of recurrence the lung has to stick up against the denuded/chemically treated pleura. With increased pain, poor inspiratory effort and atelectasis etc. this result becomes harder to achieve even with a chest drain on low suction.
Alternatively, if the operation is performed at two separate sittings then it is important that the anaesthetist is aware not to exert high ventilatory pressures to the contralateral lung. They should be using a dual lumen endo-tracheal tube so it is possible to only Valsalva the lung which has undergone the surgery at the end of the procedure to re-expand the lung.
-
Pleural abrasion, pleurectomy or chemical pleurodesis?
| Chemical pleurodesis | Pleural abrasion | Pleurectomy (Apical) |
| Recurrence rate
Lowest (1%) |
Recurrence rate
Highest |
Recurrence rate
(<5%) |
| Talc is the most effective agent sclerosant available | Least likely to be effective – parietal pleura could reform without lung sticking | Also effective without using an agent such as talc |
| Extremely easy and quick | Easy and safe, less painful | Slightly more time consuming |
| Aerolised talc can be performed through 5mm port | Can be used in conjunction with talc | Needs the most expertise
i.e. avoiding stellate ganglion and great vessels, intercostals and internal mammary artery. |
| Concerns about use of talc. ?litigation | ↓risk of haemothorax | ↑ risk of haemothorax |
| Further surgery – difficult | Can be targeted to upper parietal pleura where most of blebs will be |
Talc poudrage is the treatment of choice for recurrent pleural effusions in oncological patients or in spontaneous pneumothorax (typically secondary) elderly patients. Paediatric thoracic surgeons remain split as to the preferred technique. I prefer to do an apical pleurectomy as it avoids the need for talc in young patients which I still have reservations about using.
References
- MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. DOI: 10.1136/thx.2010.136986. Thorax. 2010;65 Suppl 2:ii18-31. doi: 10.1136/thx.2010.136986.
British Thoracic Society pleural disease guideline 2010. Good algorithm for management of spontaneous pneumothoraces (both primary and secondary). Not recently updated and also not aimed at children/adolescents in particular.
- Brown SGA, Ball EL, Perrin K, et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405-415. doi: 10.1056/NEJMoa1910775.
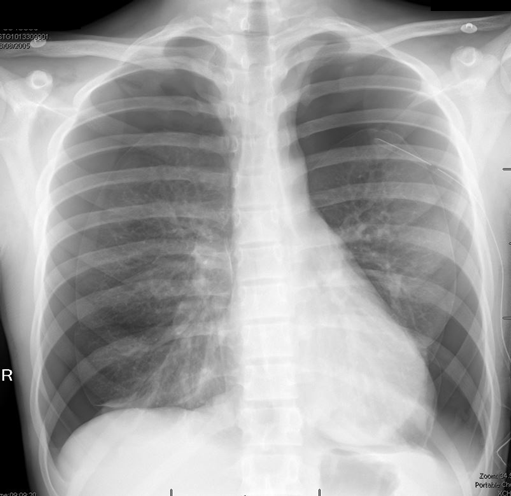
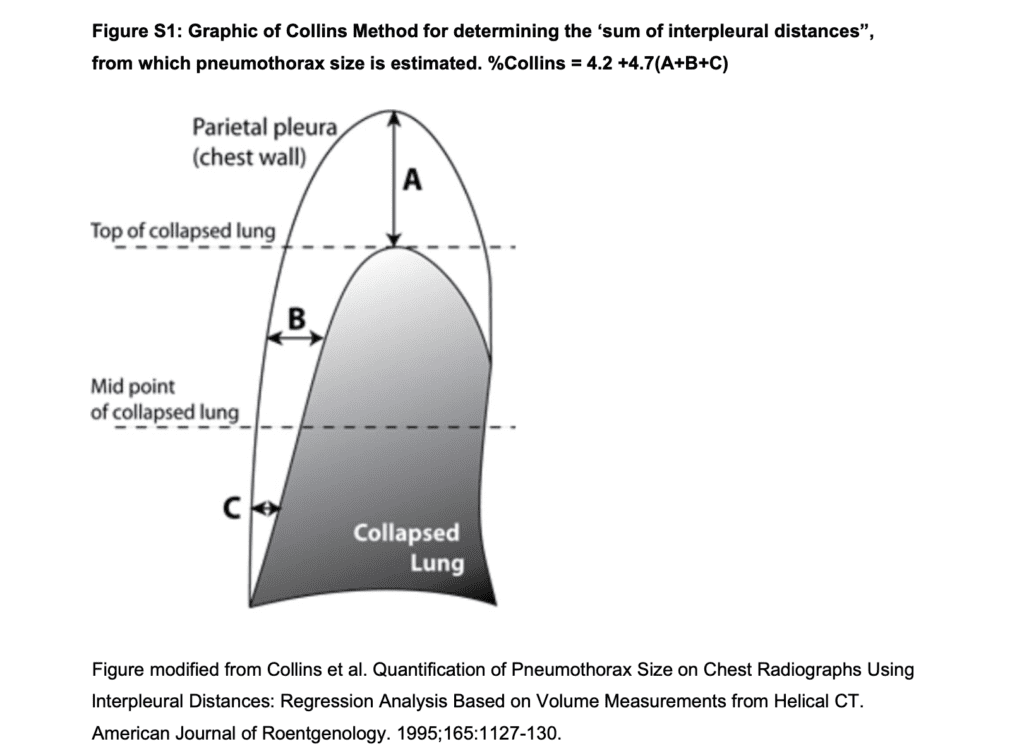
Level 1 evidence: RCT. Australian and NZ study. 316 patients (14-50 years) who had spontaneous PTx. PTx had to be 32% or larger by the method of Collins, that is the sum of the inter-pleural distances (A+B+C) of 6cm or greater. These are significant PTx that would normally be drained according to BTS guidelines or by most clinicians. 154 patients randomly assigned to immediate intervention (aspiration or drain), 162 patients to the conservative-management (oxygen and analgesia only) group. 137 (85%) in the conservative-management arm did not undergo any intervention. The recurrence rate within the 1st year in the whole cohort was low at only 39/308(13%).
The RCT provides evidence that conservative management of PSP was non-inferior to interventional management – Well worth a read.
- Leys CM, Hirschl RB, Kohler JE, et al. (Midwest Pediatric Surgery Consortium MWPSC). Changing the paradigm for management of pediatric primary spontaneous pneumothorax: a simple aspiration test predicts need for operation. J Pediatr Surg. 2020 Jan,55(1):169-175. doi: 10.1016/j.jpedsurg.2019.09.043.Epub 2019 Oct 24.
Level 3 evidence: Prospective pilot study. 33 patients treated from March 2016-March 2018 with a primary spontaneous untilateral PTx that warranted intervention. Aged 12-17.
- Laituri CA, Valusek PA, Rivard DC, Garey CL, Ostlie DJ, Snyder CL, St Peter SD. The utility of computed tomography in the management of patients with spontaneous pneumothorax. J Pediatr Surg. 2011;46(8):1523-5. doi: 10.1016/j.jpedsurg.2011.01.002.
Level 4 evidence: Retrospective case series by Kansas City group. 34 children with spontaneous PTx, 26 patients had a preoperative CT scan. 8 patients (8/26 – 30%) had blebs visible on CT scan. 18 patients had negative scans, 14 of these patients (14/18 – 78%) were found to have blebs at surgery. The sensitivity of the CT scan for identifying blebs was only 36%.
- Miscia ME, Lauriti G, Lisi G, Riccio A, Lelli Chiesa P. Management of spontaneous pneumothorax in children: a systematic review and meta-analysis. Eur J Pediatr Surg. 2020;30(1):2-12. doi:10.1055/s-0039-3402522
A Meta-analysis based of purely paediatric spontaneous pneumothoraces. Analysis based on 23 studies and 16 with quantitive data. All studies were of retrospective nature so the quality of any conclusions is limited.
- Sim SKR, Nah SA, Loh AHP, Ong LY, Chen Y. Mechanical versus chemical pleurodesis after bullectomy for primary spontaneous pneumothorax: a systemic review and meta-analysis [published online ahead of print, 2019 Oct 10]. Eur J Pediatr Surg. 2019;10.1055/s-0039-1697959. doi:10.1055/s-0039-1697959
A meta-analysis on chemical versus mechanical pleurodesis. Based on 7 studies – 1 RCT and 6 observational cohort studies, 1,032 cases. Chemical pleurodesis had a significantly lower recurrence rate 1.2% versus 4.0% for mechanical pleurodesis (p = 0.0007).