National Lines Survey (2019-22)


This has now been completed and the results presented at #69th BAPS, (Bruges 2023), with the senior being Mr Paul Farrelly (Manchester) with Sophie Lewis (Liverpool), Sharif Baqer (Manchester), and Rachel Harwood (Liverpool) among the authors.
Abstracts:
-
Working towards a National Standard in Paediatric Central Vascular Access – Where are we now? – A BAPS Approved National Survey
Aim: A large cohort of paediatric patients require central vascular access. A variety of devices are available and there are various techniques to insert and manage these devices. Our aim is to assess the current demographic of clinical practice across multiple centres within the UK and Ireland.
Methods: An online questionnaire was distributed to all BAPS members. Our target audience included healthcare professionals involved with inserting central vascular access.
Results:
- There was a total of 59 responses representing 19/27 paediatric surgery tertiary centres within the UK. Most respondents were paediatric surgeons (45/59). Respondents were asked if their department had a designated vascular access service with only 6/19 centres reporting a resounding yes.
- The preferred insertion method was percutaneous insertion with ultrasound (US) guidance at 86% (51/59) but 31% (16/51) reported this would be dependent on the weight of the child with the median average weight cut off reported as 2.5KG (range 1KG to 10KG). 52/59 responded fluoroscopy was routinely used, but the use of contrast and placing the patient in a neutral position was more varied.
- The most reported line complication was line failure requiring re-do and with most clinicians referencing a risk of 1 in 100. The risk of death was quoted on average 1 in 10,000.
Conclusion: Percutaneous insertion under US guidance and fluoroscopy is becoming the gold standard. However, services across the country are variable and further work is required at a national level to standardise care.
-
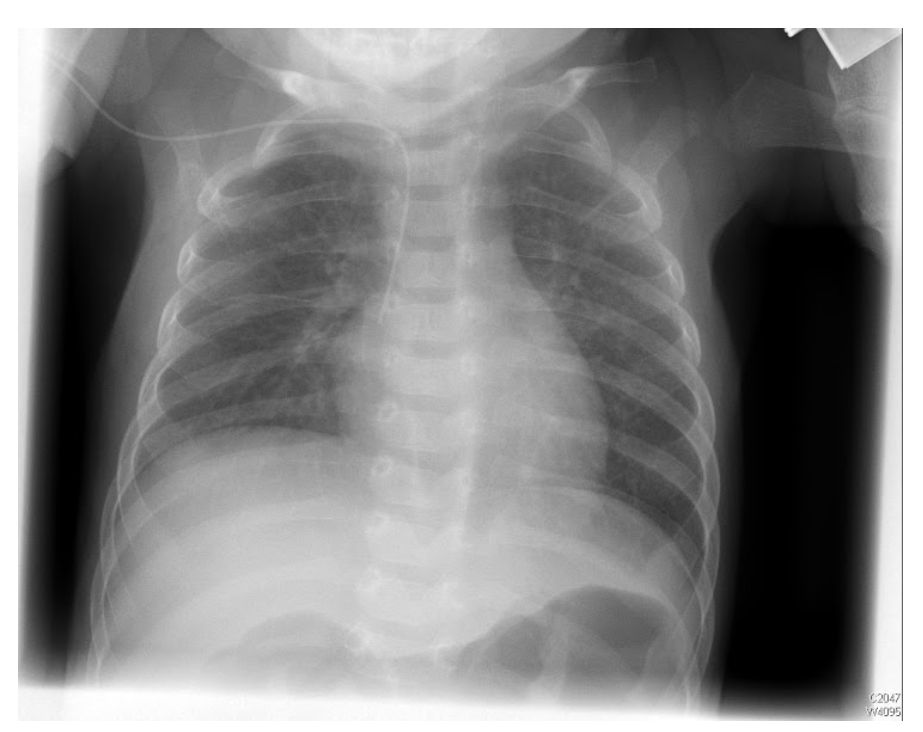
Paediatric Central Line Tip Position: Do We Agree?
Aim: To assess what clinicians consider optimal and acceptable tip position for various forms of CVA and reliability in interpretation of tip position on radiographs.
Methods: An online questionnaire was distributed to all BAPS members following a pilot study with the Paediatric Surgery Trainee Research Network. Respondents were asked their opinion on acceptable and optimal line tip position and to comment on tip position and safety of use on ten chest radiographs.
Results:
- There was a total of 59 responses representing 20/27 paediatric surgery tertiary centres in the UK and Ireland. The majority of respondents reported the optimum position as SVC/RA junction for tunnelled central lines and PICC lines but “just into the right atrium” for haemodialysis lines.
- There is variability in the radiographical landmark used as the closest correlation to the SVC/RA. The majority used the 2nd vertebral body below the carina (35.6%)
- Fleiss Kappa demonstrated only moderate agreement (0.48) in terms of tip position and poor agreement (0.33) in whether the line was safe to used.
Conclusion: There is significant variability in clinician assessment of anatomical central line tip position and what constitutes a safe tip position. Recent studies which reviewed CT scans show strong evidence for the use of position in relation to vertebral bodies below the carina. No nationally accepted guidelines exist. It is vital to work towards a national consensus on the ideal tip position and how we interpret tip position to minimise potential complications.
Curated by Prof. Mark Davenport
March 2025